Binge Eating Disorder (BED) is a complex mental health condition characterized by recurrent episodes of excessive eating and a sense of loss of control. Recognizing BED involves understanding its key signs, including guilt, loss of control, and recurring patterns impacting daily life. The disorder is closely linked to depression and anxiety, with neurological changes triggering intense cravings. Effective treatment combines cognitive-behavioral therapy (CBT), interpersonal therapy, mindfulness-based interventions, and support groups to address negative thought patterns, improve relationships, and foster a healthier relationship with food and bodies. Self-care practices such as regular physical activity, balanced diets, and mindfulness are crucial alongside professional therapy for successful BED management.
Binge eating disorder (BED) is a complex condition characterized by recurrent episodes of uncontrollable eating, often leading to significant distress and negative consequences. Beyond the obvious effects on physical health, BED is deeply intertwined with depression, exacerbating an already challenging mental state. This article delves into understanding BED, recognizing its subtle signs, exploring therapy options, and emphasizing the importance of support systems for effective recovery and management.
- Understanding Binge Eating Disorder: Unraveling the Complex Condition
- Recognizing the Signs and Symptoms: A Comprehensive Guide
- The Connection Between Depression and Binge Eating
- Therapy Approaches for Binge Eating Disorder: Effective Strategies
- Cognitive Behavioral Therapy (CBT): A Step-by-Step Breakdown
- Support Systems and Self-Care for Recovery and Management
Understanding Binge Eating Disorder: Unraveling the Complex Condition
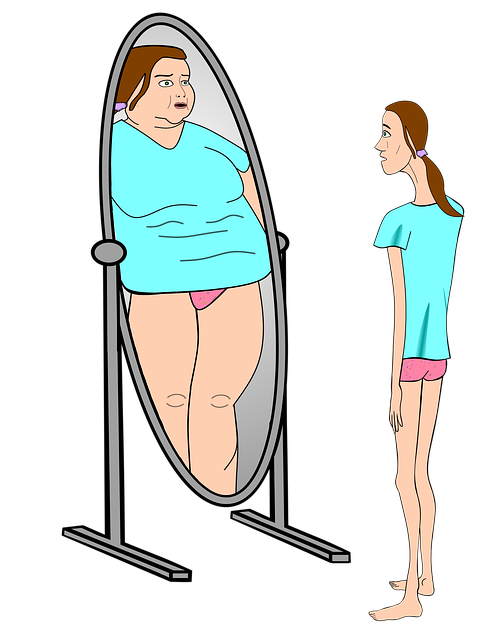
Binge eating disorder (BED) is a complex and often misunderstood condition characterized by recurrent episodes of excessive eating, accompanied by a sense of loss of control. It goes beyond casual overeating; individuals with BED experience intense urges to consume large quantities of food, even when they are not physically hungry. This compulsive behavior typically leads to feelings of shame, guilt, and distress following the binge. The disorder is more than just a lack of willpower; it’s a deep-rooted issue that can stem from various factors, including emotional distress, hormonal imbalances, or underlying mental health conditions.
The complex nature of BED means it often co-occurs with depression, anxiety, and other mood disorders, making the road to recovery more challenging. Unraveling this intricate condition involves a comprehensive approach to therapy. Cognitive-behavioral therapy (CBT), for instance, helps individuals identify and change negative thought patterns and behaviors related to food. Interpersonal therapy focuses on improving relationships and social skills, addressing issues that may contribute to emotional eating. Additionally, mindfulness-based interventions are gaining traction for their ability to help individuals develop a healthier relationship with food and their bodies.
Recognizing the Signs and Symptoms: A Comprehensive Guide
Recognizing the signs and symptoms of binge eating disorder (BED) is crucial for seeking timely intervention and support. BED is characterized by episodes of excessive eating, often leading to feelings of guilt or distress afterward. Individuals with BED may experience a loss of control over their eating habits, consuming large quantities of food in a short period, even when they are not physically hungry. This disorder goes beyond occasional overeating; it involves a recurring pattern that significantly impacts an individual’s life.
Beyond the obvious physical indicators, depression and low mood are often closely linked to BED. Emotional distress, such as stress, anxiety, or sadness, can trigger binge-eating episodes. Individuals may use food as a coping mechanism, temporarily alleviating negative emotions but ultimately exacerbating them due to feelings of shame and guilt. Recognizing these patterns and understanding the complex interplay between eating behaviors and mental health is essential for effective treatment and recovery.
The Connection Between Depression and Binge Eating
Depression and binge eating disorder are closely linked, forming a complex relationship that can significantly impact an individual’s overall well-being. Research indicates that individuals with depression are at a higher risk of developing binge eating disorder, and vice versa. This connection is not merely coincidental; it delves into the neurological aspects of these conditions.
When an individual experiences depression, their brain chemistry may alter, leading to imbalanced levels of neurotransmitters like serotonin and dopamine. These neurotransmitters play a crucial role in regulating appetite, pleasure, and mood. As a result, people with depression might find themselves grappling with intense cravings and loss of control over eating habits, which are characteristic symptoms of binge eating disorder. Understanding this relationship is essential in developing comprehensive therapy approaches that address both depression and binge eating effectively.
Therapy Approaches for Binge Eating Disorder: Effective Strategies
Treatment for binge eating disorder (BED) often involves a combination of approaches tailored to address both the psychological and behavioral aspects of the condition. Cognitive-behavioral therapy (CBT) is a widely recognized and effective strategy. It helps individuals identify and change negative thought patterns related to food, improving their relationship with meals. CBT also teaches coping mechanisms to manage impulsive eating behaviors. Through this process, patients gain better control over their eating habits and learn to recognize triggers for binge episodes.
Another powerful tool is interpersonal therapy (IPT), focusing on relationships and social factors contributing to BED. By exploring and enhancing communication skills, individuals can improve their overall well-being, which positively impacts eating behaviors. Additionally, mindfulness-based interventions have shown promise in treating BED by promoting present-moment awareness and helping individuals recognize hunger cues, thus reducing binge episodes. These therapy approaches offer comprehensive strategies to help those with BED develop healthier coping mechanisms and improve both their mental health and relationship dynamics.
Cognitive Behavioral Therapy (CBT): A Step-by-Step Breakdown
Cognitive Behavioral Therapy (CBT) is a highly effective approach for managing binge eating disorder (BED). The therapy focuses on identifying and changing negative thought patterns and behaviors that contribute to overeating and depression. Here’s a step-by-step breakdown:
1. Assessment and Education: Therapists begin by evaluating the client’s history, symptoms, and triggers for binging. They educate the individual about BED, its causes, and how it interacts with co-occurring depression. This knowledge empowers clients to understand their condition better.
2. Cognitive Restructuring: This involves challenging and modifying distorted thinking patterns. For instance, a client might believe, “I’m a failure if I don’t eat everything on my plate.” CBT helps replace this thought with a more realistic perspective: “It’s okay to stop eating when I feel full, and I deserve self-compassion regardless of my food choices.”
3. Behavioral Activation: CBT encourages clients to engage in activities that bring pleasure and fulfillment outside of food. This can involve pursuing hobbies, social interactions, or exercise, helping individuals find healthier ways to manage their emotions.
4. Mindfulness Techniques: Learning mindfulness helps individuals become more aware of their feelings, thoughts, and physical sensations without judgment. This awareness allows them to recognize early signs of binge-eating urges and implement coping strategies before behaviors escalate.
Support Systems and Self-Care for Recovery and Management
Having a strong support system is vital for managing binge eating disorder (BED). Family, friends, and peers can play a significant role in recovery by offering emotional support, understanding, and encouragement. They can help individuals with BED stay accountable, provide comfort during challenging times, and celebrate successes. Support groups are also beneficial, as they connect individuals with others facing similar struggles, fostering a sense of belonging and shared experience. This network ensures individuals don’t feel isolated in their battle against BED.
Self-care practices are essential alongside professional therapy for effective BED management. Engaging in regular physical activity, maintaining a balanced diet, and practicing mindfulness can help regulate emotions, reduce stress, and manage eating urges. Adequate sleep, relaxation techniques, and setting boundaries to protect personal time are also crucial. By prioritizing self-care, individuals with BED can develop healthier coping mechanisms, improve overall well-being, and enhance their ability to stick to treatment plans.
Binge eating disorder is a complex condition that often intersects with depression, highlighting the importance of integrated therapy approaches. By recognizing signs early and leveraging effective strategies like Cognitive Behavioral Therapy (CBT), individuals can navigate their recovery journey with support systems and self-care practices tailored to their unique needs. Understanding these interconnected elements empowers those affected to reclaim control over their mental health and overall well-being.